Diabetes mellitus, or as it is commonly referred to simply as diabetes, is a condition in which blood sugar (glucose) levels are abnormally high due to the body’s inadequate insulin production or inappropriate target organ response (insulin resistance). This disorder has emerged as a significant public health issue worldwide. Over the past 30 years, the number of cases has quadrupled to over 830 million in 2022, affecting around 14% of adults worldwide, according to the World Health Organization (WHO) data.
Receiving a diagnosis of diabetes mellitus can be daunting and overwhelming. This article explains why the condition develops, its implications for long-term health, and prevention measures you can take.
Understanding Diabetes: Causes, Effects, and Prevention Tactic
What is diabetes mellitus, and what causes it?
Diabetes mellitus is characterized by abnormally high blood sugar (glucose) levels. This may be caused by the body’s inability to produce enough insulin or by improper target organ response. Insulin is a hormone created by the pancreas, an organ in the abdomen that converts food into energy, aids digestion, and regulates blood sugar levels. Inappropriate target organ response means insulin resistance: even with normal insulin levels, tissues do not respond well, i.e., they do not absorb glucose from the blood.
When you eat or drink, the food gets broken down into different components, including glucose, a primary energy source. As glucose enters your bloodstream, it tells the pancreas to release insulin. Insulin then helps move sugar from your blood into your cells, turning it into energy. You can use this energy immediately or store it as fat or glycogen for later.
Throughout the day, the blood sugar level naturally goes up and down. It typically rises after meals and returns to normal within about two hours, thanks to insulin. Once the blood sugar level returns to normal, insulin production slows down. Normal blood sugar levels hover between 3.9-5.6 mmol/L for most people. However, eating a lot of carbohydrates can spike blood sugar levels. If the body doesn’t produce enough insulin to help get that sugar into the cells, it can lead to high blood sugar levels. This imbalance can cause the symptoms and complications linked to diabetes.
There are two types of diabetes, which are classified based on how the body produces or uses insulin:
- Type 1 diabetes, also known as juvenile or insulin-dependent diabetes, is a condition in which the pancreas doesn’t produce enough insulin or sometimes none at all. This could be due to an autoimmune reaction, in which the body mistakenly attacks its tissues. It’s a chronic condition, which means it’s something that people can manage over time, and with the proper support and care, they can lead full and active lives!
- Type 2 diabetes is the most common type and usually affects adults. It happens when the body either doesn’t respond well to insulin or doesn’t make enough of it. Having blood sugar levels that are higher than usual but not high enough to be classified as type 2 diabetes is known as prediabetes.
What are the main risk factors?
Type 1 diabetes is a condition that cannot be prevented or treated at this stage of medical knowledge.
Known risk factors include:
- Family history: Having a parent, brother, or sister with type 1 diabetes.
- Genetics: Certain genes can increase the risk of developing type 1 diabetes.
- Geography: The incidence of type 1 diabetes tends to be higher further away from the equator.
- Age: It usually develops in children and teens, but it is also possible to get it in adulthood.
Type 2 diabetes and prediabetes share almost all of the same risk factors. If you already have prediabetes, this is an added risk factor that makes you more likely to develop type 2 diabetes.
The main risk factors include:
- Family history: Having first-degree relatives (parent, sister, brother, son, daughter) involved with this condition.
- Geography: Preveilance is more significant among people of specific geographic locations or their descendants, such as those of Hispanic, African, and Asian descent.
- Lack of physical activity and unhealthy eating habits: Eating more sweets and “white” carbohydrates (white bread, rolls, anything made from white flour) and drinking sugary drinks (soft drinks, juices, too much sugar in coffee, tea) may put you at higher risk. While regular sports and fitness activities can decrease the risk.
- Obesity: This factor is closely related to lifestyle habits. Those who consume more calories than they need without exercising will gain weight, eventually increasing the risk. However, it is important to note that obesity can be a result of hormonal imbalance and requires medical evaluation.
Gestational diabetes: Some women may develop diabetes during pregnancy, even if they did not have it before. In 2021, it affected 15% of pregnant women in Europe and 12.8 percent in Hungary. This condition is caused by hormones that can make insulin less effective, leading to insulin resistance. It usually resolves after childbirth; however, it slightly increases the risk of developing diabetes later in life.
How is diabetes diagnosed?
The diagnosis of diabetes mellitus is based on a combination of symptoms and the results of blood tests.
Recognize the symptoms:
Many people with type 2 diabetes may not experience any symptoms at all. For those who do, the most common symptoms include:
- Frequent urination
- Increased thirst
- Blurred vision
- Unintended weight loss
Type 1 diabetes can develop suddenly, while type 2 diabetes typically progresses more gradually. This gradual onset can lead to symptoms being overlooked. It is crucial to remain vigilant and recognize any changes in your health, as early intervention can make a significant difference.
Regular screening with laboratory tests:
Diabetes can be identified through specific laboratory tests:
- Random Blood Sugar Test: In this test, blood can be drawn at any time, regardless of when you last ate. If your blood sugar level is 11.1 mmol/L (200 mg/dL) or higher and you exhibit symptoms of high blood sugar, this confirms a diagnosis of diabetes mellitus.
- Fasting Blood Sugar Test: This test is conducted after fasting for 8 to 12 hours, usually overnight. An average fasting blood sugar level is less than 5.55 mmol/L (100 mg/dL). A fasting blood sugar level of 7.0 mmol/L (126 mg/dL) or higher may indicate diabetes.
- Hemoglobin A1C Test (A1C): The A1C blood test measures the average blood sugar level over the past two to three months. Typical A1C values range from 4 to 6 percent. An A1C level higher than 6.5 percent may indicate diabetes.
- Oral Glucose Tolerance Test (OGTT): The patient is tested for blood sugar before and 2 hours after drinking a solution containing 75 grams of sugar. This test is typically performed when other basic tests do not provide a clear diagnosis.
It is important to note that the blood tests must be repeated on a different day to confirm that the results remain abnormally high.
What are the long-term complications?
If not properly managed, diabetes can lead to severe complications due to the narrowing of blood vessels caused by prolonged high sugar levels. This narrowing reduces blood flow to various parts of the body. Over time, elevated blood sugar and poor circulation can damage the heart, brain, eyes, kidneys, nerves, and skin. As a result, it may lead to developing conditions such as angina, heart failure, stroke, vision impairment, kidney failure, neuropathy (nerve damage), and slow-healing skin ulcers since the immune system is also compromised.
Diabetes can be prevented and managed by a healthy lifestyle, regular screening
Although certain risk factors, such as genetics, family history, age, and ethnicity, cannot be changed, you can take important measures to prevent or manage diabetes:
-
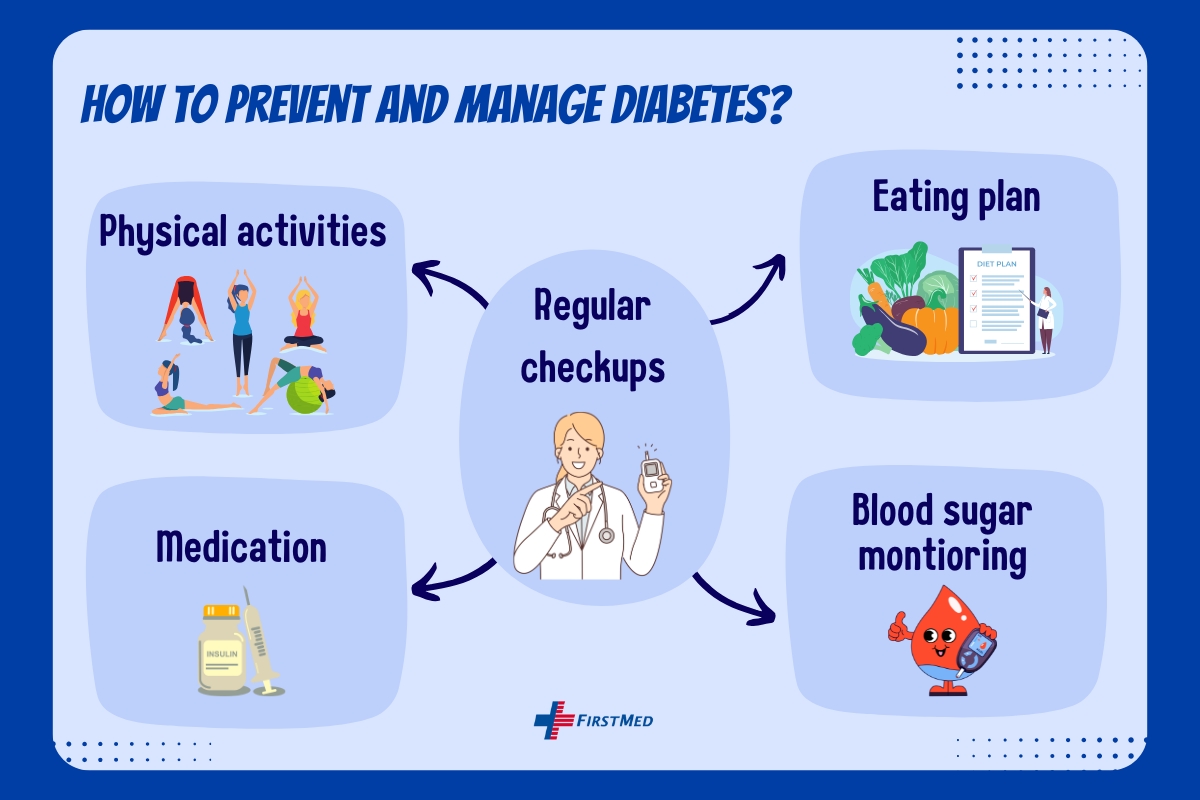
The primary goal of treatment is to maintain glucose levels as close to normal as possible to prevent or postpone complications. Type 2 diabetes can often be effectively controlled or even reversed through a special diet and regular exercise.
- Managing blood sugar levels strictly decreases the likelihood of developing complications. If you have or are at risk of diabetes, monitor blood sugar at home and schedule visits with a doctor every 3-4 months, even if blood sugar levels appear well controlled.
- Additionally, it is vital to regularly test for and treat high blood pressure and elevated cholesterol levels, as managing these can also help prevent complications. Yearly monitoring heart health, kidney function, and eye and foot health is also crucial.
- Medications can effectively manage diabetes by helping regulate blood sugar levels, improve insulin sensitivity, and prevent complications associated with the condition. These treatments may include oral medications, insulin injections, and other therapeutic options tailored to our patients’ specific needs.
Optimal care requires a long-term relationship with your doctor. Be motivated and adhere to treatment and monitoring recommendations to significantly enhance your long-term outlook.
Diabetic care at FirstMed
At FirstMed, we take a holistic approach to help our patients prevent and manage diabetes. We focus on helping them understand their condition and educating them about the necessary lifestyle changes and their importance. We aim to make the process of adopting these lifestyle changes as stress-free as possible. We also acknowledge that the fast pace and demands of modern life can make it challenging for some patients to receive regular care.
Our team of general practitioners, pediatricians, and specialists collaborates to diagnose and treat children and adults with diabetes while focusing on preventive medicine. Patients receive comprehensive health screenings, such as Annual Health Maintenance Exams and Well-Child Checks, where we assess risk factors and conduct relevant laboratory tests on the same day. If needed, our doctors will recommend diet, exercise, and self-monitoring of blood sugar levels and blood pressure. You will also have the opportunity to ask any questions you may have.
Our doctor may recommend appropriate therapies and refer you to a specialist for further evaluation. They will also provide guidance on monitoring blood sugar levels at home if necessary. Additionally, we will establish a regular check-up schedule to help you stay on track with managing this condition, including sending reminders for upcoming appointments.
Regular screenings are essential for safeguarding your health. You can effectively prevent severe complications and lead a healthier life by making timely lifestyle changes.
First published: March 8, 2013 / Updated: November 14, 2024




